Pharmacy
Oklahoma Complete Health is committed to providing appropriate, high-quality, and cost-effective drug therapy to all Oklahoma Complete Health members. Oklahoma Complete Health covers prescription medications and certain over-the-counter medications with a written order from an Oklahoma Complete Health provider. The pharmacy program does not cover all medications. Some medications may require prior authorization, and some may have limitations. Other medically necessary pharmacy services are covered as well. Oklahoma Complete Health follows the State of Oklahoma’s preferred drug and prior authorization criteria.
Use our Medicaid Preferred Drug List to find more information on the drugs that are covered.
Please refer to https://oklahoma.gov/ohca/providers/types/pharmacy/pharmacy.html for the most up-to-date lists of brand required medications, covered over-the-counter products, and diabetics supplies.
Please refer here: https://oklahoma.gov/ohca/providers/types/pharmacy/prior-authorization/2025.html for 2025 clinical criteria regarding medications needing prior authorizations.
If your pharmacy is experiencing a rejection & need an immediate override, please call our pharmacy helpdesks (open 24/7) at 1-833-750-3660 (SoonerSelect) or 1-833-750-3682 (Children's Specialty Plan). Please reach out directly to our local pharmacy team at oklahoma_complete_health_pharmacy@centene.com regarding general pharmacy questions or escalations.
Medication Prior Auth Search
Please utilize our Preferred Drug List posted above or our search tool function to determine if a medication requires a prior authorization, which tier the medication is in, or if the medication has step therapy, age, or quantity limits
Express Scripts, Oklahoma Complete Health’s PBM, processes pharmacy claims and supports pharmacy enrollment in our network. Information to contact Express Scripts for pharmacy enrollment is available online at this link: https://www.esiprovider.com/ This is an external link that will take you outside the Oklahoma Complete Health website.
For Application Assistance, Document Inquiries or if you have questions in regards to filling out your online application, please contact Express-Scripts at PBMProviderOperations@express-scripts.com.
Please include your pharmacy’s NCPDP in the email subject line.
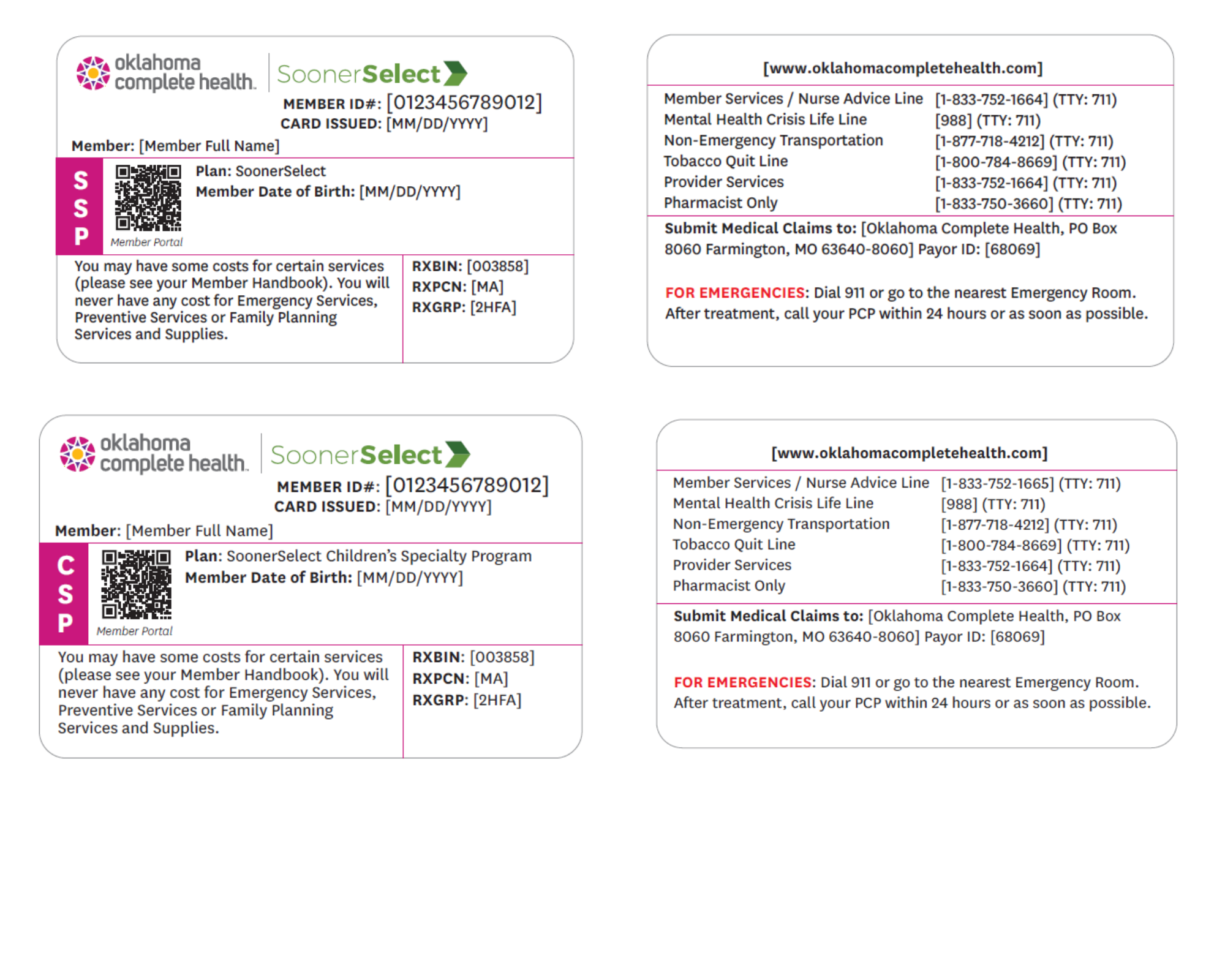
Pharmacy Processing Information:
RxBIN 003858
RxPCN MA
RxGroup 2HFA
ID Numbers will remain the same as Medicaid ID#
Maximum Allowable Cost Pricing Information
Pharmacies across Express Scripts pharmacy network can log into ESI’s portal for MAC pricing information
https://prc.express-scripts.com/frontend/prcportal/#/index
Pharmacy Services reviews prior authorizations. CoverMyMeds is the fastest and easiest way to review, complete and track PA requests. Our electronic prior authorization (ePA) solution is HIPAA-compliant and available at no cost to providers and their staff.
To use COVER My MEDs please see: https://www.covermymeds.com/main/prior-authorization-forms/ This is an external link that will take you outside the Oklahoma Complete Health website.
OR CALL 1-833-331-1515 (SoonerSelect) or 1-833-655-0896 (SoonerSelect Children’s Specialty Program)
Prior Authorization Request Form for Most Prescription Medications (PDF)
Step Therapy Exception Request Form (PDF)
Prior Authorization Request Form- Atypical Antipsychotics for Children under the age of 5 (PDF)
Prior Authorization Request Form- Stimulants for Children under the age of 5 (PDF)
Check if CPT code requires authorization – https://www.oklahomacompletehealth.com/providers/preauth-check.html
Submit prior authorization via Availity-https://www.availity.com/essentials
Members may receive up to a 90-Day supply of certain maintenance medications pursuant to the State of Oklahoma’s maintenance drug program.
Maintenance Medications Up to 90 Days. link: https://oklahoma.gov/ohca/providers/types/pharmacy/maintenance-drug-list.html This is an external link that will take you outside the Oklahoma Complete Health website.
To find a pharmacy that is in the Oklahoma Complete Health network, you can use the Find a Provider tool
Specialty drugs used to treat complex, chronic conditions are generally filled at specialty pharmacies due to the storage, handling and requirements to dispense them. Pharmacies who accept all terms and conditions of these products and of our network may dispense these drugs. OHCA has implemented a limited specialty network for hemophilia. Pharmacies who would like to be considered in network for hemophilia will need to contact OHCA.
To protect the health of our members, Oklahoma Complete Health has a pharmacy lock-in program. This is for members who abuse or misuse prescription drugs. Members are assigned to one pharmacy and one doctor. Members may change your doctor or pharmacy one time a year unless you have a special situation like moving. If members are placed in the program, they may be enrolled for a minimum of two years. We will review enrollment at least every year. Members and providers also have the option to appeal being placed in the lock-in program.
Historically there have been some over the counter products on the state's formulary; however, pharmacies don't always have them in stock or the products our members need aren't covered. Therefore, we have implemented an Over-the-Counter Product Value Add Benefit. The benefit is $30 per member per quarter. Our members can view the full catalog of items on our website and can order online (cvs.com/benefits), by phone (1-888-628-2770 (TTY 711), or pick up at any CVS Pharmacy.
Certain DME supplies are medical benefit only. If your pharmacy wishes to dispense DME supplies (nebulizers, etc.) via medical benefit, please contract with our plan by completing the contract request form found here: https://www.oklahomacompletehealth.com/providers/become-a-provider.html
Oklahoma Complete Health is expanding the prescription benefit to improve access to care. Beginning April 1, 2025, medications across five (5) drug classes will not count towards the member’s monthly six (6) prescription limit.
The drug classes are as follows and include more than 500 medications.
Systemic Antibiotics and Antivirals
Anticonvulsants
Behavioral Health Medications
Cardiovascular Medications
Diabetic Therapies
This prescription enhancement will help reduce ER visits and readmissions, while lowering members’ out-of-pocket costs and reducing wait times for medication refills.
For claims processing assistance, please call our pharmacy helpdesks (open 24/7) at 1-833-750-3660 (SoonerSelect) or 1-833-750-3682 (Children's Specialty Plan).
General questions or escalations can be directed to: oklahoma_complete_health_pharmacy@centene.com
Example ID Cards
Please call member, provider, or pharmacy services for all patient related inquiries. Phone numbers differ for Sooner Select (SSP) and Children's Specialty Programs (CSP). Important numbers can be found on the back of your member ID Card.